

20 seconds or is it contained within one large square on the readout? The answer is no, because it's variable and there are no P-waves.

Which is why, instead of a P-wave, atrial flutter will produce flutter, or F-waves. 1 Hemodynamically unstable patients with AFl should receive synchronized electrical cardioversion.Pro Tip #1: Due to this erratic electrical activity, the normal function of the SA node is usually suppressed and noneffective. 4 If rhythm identification is unclear and the patient is stable, adenosine or Valsalva maneuver may be employed to slow conduction through the AV node such that the atrial flutter waves are more readily apparent.
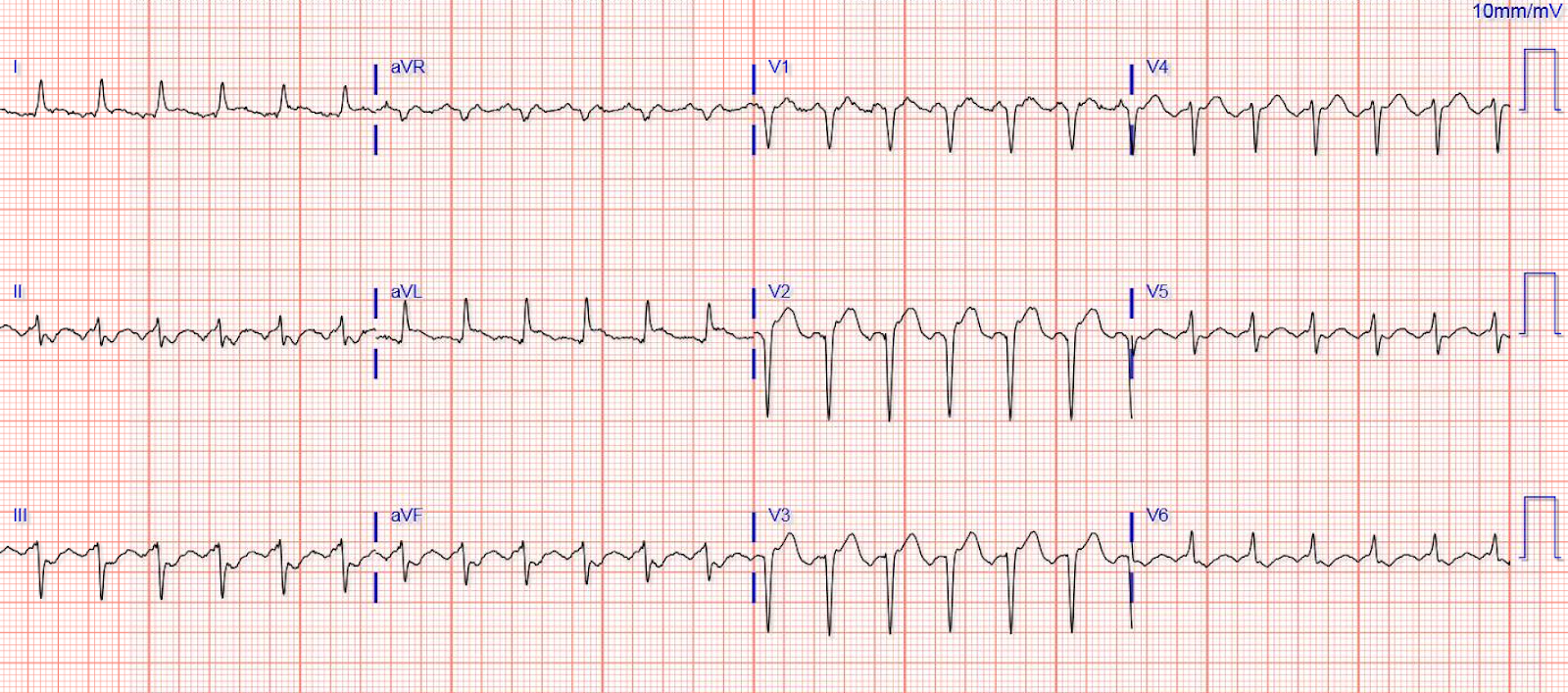
The initial treatment for AFl focuses on rate control of the ventricular response with AV nodal blocking agents such as beta-blockers and calcium channel blockers. Common symptoms of AFl include palpitations, light-headedness, fatigue, presyncope, mild shortness of breath, and possibly chest pain or hypotension. 1 Risk factors for AFl include presence of heart failure, chronic obstructive pulmonary disease, antiarrhythmic medications, thyrotoxicosis, pulmonary embolism, prior cardiac surgery or prior atrial ablation. The underlying mechanism of type II AFl is unclear. 3 The ECG in atypical (type II) AFl is characterized by upright F waves in leads II, III, aVF, and V 6 and by biphasic F waves in leads I, aVL, and V 1. 2 Type I AFl is most commonly caused by the presence of a macro-reentrant circuit in the right atrium that includes a small strip of tissue between the inferior vena cava and the tricuspid annulus known as the cavotricuspid isthmus. 1 The ECG in type I (typical) AFl is characterized by an inverted sawtooth flutter (F) wave pattern in the inferior leads II, III, and aVF, low amplitude biphasic F waves in leads I and aVL, an upright F wave in precordial lead V 1, and an inverted F wave in lead V 6. Atrial flutter (AFl) is a cardiac dysrhythmia characterized by rapid and regular depolarization of the atria that appears as a sawtooth pattern on the electrocardiogram (ECG) and is categorized into type I (typical) and type II (atypical) AFl.


 0 kommentar(er)
0 kommentar(er)
